Everyday Foot Care
Our feet are arguably one of the most important parts of the body. When it comes to health and beauty routines, the feet and toenails are usually ignored. You should always practice proper footcare to avoid any fungal infections or ailments that can not only ruin the appearance of your feet, but also cause pain. Ignoring any foot problems could potentially lead to an expensive doctor’s visit.
The most important step in proper foot care is to wash your feet daily. You should wash them with soap and water. Doing this will cleanse your feet of dirt, sweat and bacteria. It is crucial that you clean between the toes and pat your feet dry with a towel afterward. Your toenails are also an important part of the feet and you may find that they get dirtier in the summer when you wear sandals. It is important that you practice proper toenail care in addition to cleaning the rest of your feet. When trimming your nails, you should always trim straight across instead of in a rounded shape. Trimming in a curved shape may lead to ingrown toenails.
Moisturization is also important for foot care, and you should be moisturizing your feet every day. The best way to prevent dry feet is to rub lotion or petroleum jelly on your clean feet at night and put socks over them. In the morning, your feet should be soft and moisturized.
Another crucial step in proper foot care is to wear the right shoes for whichever activity you are going to partake in. In warmer weather, you should wear shoes that allow your feet to breathe. It is best to avoid shoes such as flip-fops that do not provide arch support. Tight shoes may also be harmful, and they may even cause you to develop bunions.
If you plan on taking a shower in a public area, you should be especially careful, so you do not pick up any fungi. Showers are prone to harboring different types of bacteria and fungi. You should always wear shower shoes or flip flops when walking around in locker rooms and public showers. Avoid sharing shoes with other people because this is another way that fungus may be spread.
If you are experiencing any problems with your feet you should speak with your podiatrist to determine the best method of treatment for you.
Is There a Connection Between Poor Circulation and Toenail Fungus?

Onychomycosis, otherwise known as toenail fungus, is an infection of the toenails. This type of fungus is found in moist environments, consisting of public swimming pools, shower room floors, and locker rooms. The fungus enters the body through small cracks in the skin on the feet, and it is wise to wear appropriate shoes while in these types of areas. It is a common ailment, and generally causes no pain, although it can appear to be unsightly. The symptoms that are often associated with this condition often include yellowed nails that have become thick and brittle, and may begin to crumble. It may be more prevalent among the older population, and can be difficult to treat. Research has shown that there may be a correlation between toenail fungus and reduced blood flow, and it may help to increase circulation as part of the antidote for toenail fungus. This can be improved by consuming a healthy diet that is made up of low-fat and plant based foods, which may help overall health. Toenail fungus can be a stubborn condition, and can gradually worsen if left untreated. It is strongly advised that you consult with a podiatrist if you are afflicted with this ailment who can guide you toward the correct treatment options.
For more information about treatment, contact one of our podiatrists of PA Foot & Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact one of our offices located in Allentown, Easton, Northampton, and Chew Street in Allentown, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.
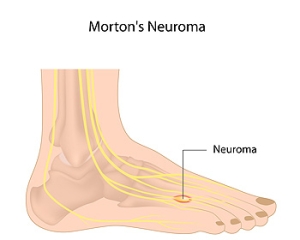
What Can Trigger Morton’s Neuroma?
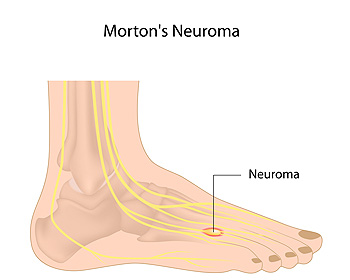 There is a nerve called the plantar digital nerve which is located between the toes. Morton’s neuroma is a condition that occurs when that nerve is irritated or squeezed and can happen from wearing shoes that do not have enough room in the toe area. When this nerve is inflamed the pressure is felt in the ball of the foot. The nerve can become thickened, and this ailment gradually becomes painful. Some of the symptoms that are associated with Morton’s neuroma can include the sensation of stepping on a pebble, the foot can feel numb, and the pain can travel between the third and fourth toes. This is a common condition among ballet dancers because of the style of dance they enjoy. There may also be existing medical conditions that can trigger Morton’s neuroma like hammertoe, bunions, and flat feet. If you have any of these symptoms please confer with a podiatrist who can guide you toward correct treatment options, which may include surgery for permanent removal of the nerve.
There is a nerve called the plantar digital nerve which is located between the toes. Morton’s neuroma is a condition that occurs when that nerve is irritated or squeezed and can happen from wearing shoes that do not have enough room in the toe area. When this nerve is inflamed the pressure is felt in the ball of the foot. The nerve can become thickened, and this ailment gradually becomes painful. Some of the symptoms that are associated with Morton’s neuroma can include the sensation of stepping on a pebble, the foot can feel numb, and the pain can travel between the third and fourth toes. This is a common condition among ballet dancers because of the style of dance they enjoy. There may also be existing medical conditions that can trigger Morton’s neuroma like hammertoe, bunions, and flat feet. If you have any of these symptoms please confer with a podiatrist who can guide you toward correct treatment options, which may include surgery for permanent removal of the nerve.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of PA Foot & Ankle Associates. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact one of our offices located in Allentown, Easton, Northampton, and Chew Street in Allentown, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Cutting Ingrown Toenails

Many individuals are affected with the foot condition known as ingrown toenails. This condition occurs when the side of the nail grows into the skin surrounding the toenail. As a result, the skin will grow overtop of the nail. This might cause pain. Many people affected with ingrown toenails are curious about how they might go about cutting an ingrown toenail. Generally, it is best to seek the help of a podiatrist to cut an ingrown toenail because doing so by oneself can potentially be damaging. If someone cuts the nail too short, they may be putting themselves at an increased risk of encouraging another ingrown toenail to develop. Also, when an inexperienced person attempts to cut an ingrown toenail, they might be increasing their susceptibility to infection. Under the care of a podiatrist, a patient can receive the care that they need to treat the underlying problem. If you have an ingrown toenail, contact a podiatrist today for an appointment.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact one of our podiatrists of PA Foot & Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact one of our offices located in Allentown, Easton, Northampton, and Chew Street in Allentown, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Different Levels of Foot Wounds

An open sore on the foot is known as a foot ulcer. It can be common among diabetic patients who have cuts on their feet, which they may not be aware of. A simple cut may develop into a foot ulcer as a result of neuropathy, which causes the inability to feel existing wounds, cuts, or scrapes on the feet. There are varying degrees of foot ulcers, which can range from a shallow wound that is on the surface to a deep wound involving the tendons and bones. Any type of wound on the foot needs prompt medical attention, and this may prevent a foot ulcer from developing. A wound on the foot is treated by cleaning out debris that may be inside of it. This is followed by tightly wrapping it with a bandage that can protect the foot, and it is beneficial to elevate it as often as possible. The more shallow the wound is, the greater the chances of a complete healing is possible. If you have a foot wound, please consult with a podiatrist who can offer the correct treatment methods for wound care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from PA Foot & Ankle Associates. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Allentown, Easton, Northampton, and Chew Street in Allentown, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
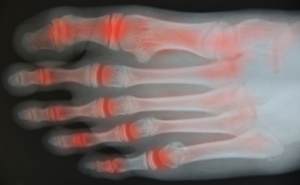
Big Toe Osteoarthritis
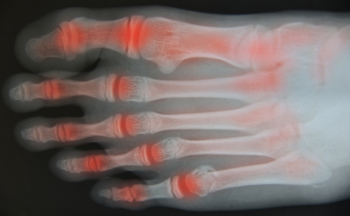
The big toe joint is one of several joints found in the foot and it is most often affected by osteoarthritis. This affliction primarily occurs in women and those who are aged 50 and above. The main symptom of this condition is pain and tenderness in the big toe that worsens when weight is put on the foot. The toe may be swollen or stiff and moving around is hampered. While there is no single reason for the development of big toe osteoarthritis, factors that may increase the risk include an injury to the toe, having gout, or being obese. It might help to wear shoes with rocker soles or rigid orthotics. It can also be beneficial to perform specific toe exercises. However, further intervention may be necessary depending on the severity of the pain. If you have pain in your big toe, it is suggested that you schedule an appointment with a podiatrist for assessment and treatment.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from PA Foot & Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact one of our offices located in Allentown, Easton, Northampton, and Chew Street in Allentown, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.